The World Health Organization recognized ageing as a disease only two years ago. Many medical professionals do not agree but there are advantages.
A Five-Minute Read
The fact that ageing had not been treated as a disease changed our attitudes towards it. We think of it as an inevitable part of life. For those trying to extend human life it was a major barrier. Hospital treatments should now change in recognition.
Extending Human Life.
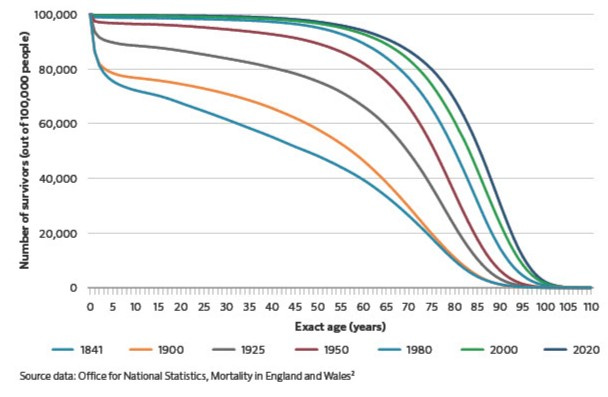
The figure shows survival charts for the UK. A single line shows the number of babies born that would live to different ages. The first line for 1841 shows the extent of child mortality. Of 100,000 babies born, nearly 25,000 died before their 10th birthday. Each successive line shows improvement. Mainly due to better nutrition, environment and medicine. The lines are marching to the right. In 1841, by the age of 45 only half of those 100,000 babies were still alive. The 2020 curve shows that half will still be alive in their late eighties. The level of child mortality in the UK is negligible today. More and more of us are living to older and older ages.
However, the end point of our journeys is not changing. There is still a finite age beyond which it is impossible to go. The oldest verified living person is Ethel Caterham. She happens to be British. She lives in Surrey and was born on August 21st, 1909. She is 115 years old. There is a growing industry trying to break that boundary. Not to allow us to live as close to the existing maximum as possible. Instead to move the maximum.
They face major scientific challenges. They need to understand the processes of ageing. They need to work out how to slow them. No one has 100 years to wait for the results of any new drug. It might take that long to prove the drug has worked. They need to develop biomarkers to show progress in much shorter periods. A recent article pointed out that “longevity” is becoming fashionable. Clinics and health spas are offering new “longevity treatments”. The problem of course is the same. How do you measure success? Even if they worked spectacularly well, how long would we have to wait to see the results?
The drug companies also faced the problem that ageing was not a recognized disease. The regulators would not authorize studies or approve drugs. Because it was not a disease it was not funded. Until WHO decision, the answer was twofold. To work on an accepted disease that is associated with ageing. The alternative was to repurpose existing drugs. Metformin, for example, created a lot of interest. Originally found in lilac it was used as a treatment for fever or snake bites in medaeval times. It is now a primary treatment for Type2 Diabetes. It also seems to slow the progression of age realated diseases.
Treating Frailty as a disease.
An article in the Financial Times this week described a new clinic in the NHS in Hull. They take the perspective that frailty is a disease. Frailty is not seen simply as part of ageing and inevitable (and untreatable). Frailty is the point where the processes of ageing interfere with everyday life. Normally such patients arrive at A&E having had a fall or some other traumatic occurrence. Instead they “capture” frail patients before something happens. The clinic brings together specialists in different parts of geriatrics. They assess a patient both psychologically and physically. They are put on an integrated treatment program. They treat frailty in “the same way that we would treat heart failure”, to quote the clinic director.
There are huge benefits for patients and the National Health Service. People who are treated in this way end up in Accident and Emergencies less often. Their numbers are down by a half compared to before the opening of the clinic a year ago. When frailty was not a disease to be treated. These people end up in hospital less. As I have argued in previous Newsletters hospitals make older people sick. They want to be at home. See Newsletter #180 Tougher Customer Journey. In the year since the clinic opened, the patients spent 72% less time in a hospital bed. Hospitals are the most expensive part of any care system. Sadly, many of those bedridden patients are the frail who have real trouble taking care of themselves.
There are problems with the disease decision
Many physicians believe that the WHO has made a mistake. There are multiple arguments. It is difficult to have a disease that everyone in the world has. This is the first. We know that the symptoms of ageing are only weakly related to chronological age. How then will the disease be defined? We know that ageism is bad for our health. Many experts believe that the disease decision will make ageism worse.
If you enjoy the Newsletter please recommend it to friends and send them to Substack to subscribe. It is free. Alternatively try the button below. All the Newsletters and lots more background is on my website thebusinessofage.com.